Dr. Carlson and his staff at Restore Health Today are experienced in treating and helping patients with RSD/CRPS. At any point through this article, should you decide that you would like a free to see whether or not you are a candidate for their treatment, simply call (801) 228-1906 and we will gladly set that up for you.
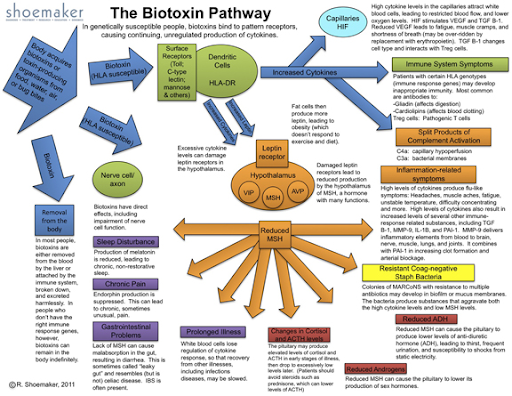
Reflex Sympathetic Dystrophy (RSD) is an autoimmune disease affecting the sympathetic nerves, so that the nerves keep firing, causing constant pain. It is probably a defect in the NMDA receptors, and more specifically a defect in the calcium channels in those receptors such that calcium ends up flooding the nerve terminals, which causes the nerves to keep firing.
The diagnosis of RSD is made clinically by ruling out other neurological and vascular causes of the pain, and then using the classical history and physical findings and the response to treatments which have been found to be effective for RSD.
The classic history of RSD: RSD usually follows some physical trauma. Usually, there is a history of significant trauma, but sometimes only minor trauma is the inciting trigger for the disorder. There is often significant swelling of the involved extremity, and the patient may have applied cold compresses for an extended period of time (which, in this case may be another contributor to the nerve dysfunction).
The pain is always moderate to severe, and out of proportion to the nature of the trauma inflicted or the general appearance of the extremity. In my experience observing patients, there is so much pain that the patient is unable to draw their attention away from the extremity (which may also contribute to the dysfunction of the normal “somatic” nervous system, and the ramping up of the sympathetic nervous system to take over the sending of pain signals from the affected extremity).
If the patient is brought into physical therapy, or otherwise increases regular use of the limb (which must be done carefully, and under supervision) early after onset of the disorder, the symptoms sometimes abate and disappear, pointing to a resumption of the normal function and healing of the somatic nervous system, and shutting down of the dysfunctional sympathetic nervous system.
RSD, in my experience, only occurs in people with autoimmune disorders themselves, or in people with a family history of autoimmune disorders. There is often a history of migraines. If this is universally true, then surgeons contemplating surgery on people with a history of autoimmune disorders should take this into account while evaluating patients and advising about whether a procedure is indicated.
It is all the more important to consider personal and family history and the risk of RSD because RSD is usually a lifelong disorder, and most people who develop it after having an elective procedure wish they had chosen not to have the procedure because of the degree of suffering they endure.
We have found that RSD is probably a migraine equivalent: all of my RSD patients have responded to one migraine treatment or another, which I will discuss below.
First I would like to present a general outline of causative factors and metabolic pathways and systems involved so that as I discuss the treatment options, the reader will be better able to organize their thoughts about prevention and treatment of this disorder.
- RSD is an autoimmune disorder and involves a confused and overactive immune system and inflammation. Any medication or supplement or lifestyle adjustment which can calm the immune system and calm inflammation can help avoid the disease and decrease its’ severity. Examples of treatment options are as follows:
- Anti-inflammatories, both pharmaceutical and non-pharmaceutical are likely to help, including Toradol in the commonly-used “Migraine Cocktail”. Prednisone can help people with cluster migraines and a subset of patients w/ RSD. Ibuprofen and other nonsteroidal anti-inflammatories also often help. Botanical / natural anti-inflammatories include circumen, bromelain, and ginger extract. A functional or integrative medicine doctor or naturopath can help with the many other natural anti-inflammatories.
- Avoid petroleum products, heavy metals, GMO grains, gluten, dairy and all other substances which are “new” to our system, and are not things our ancestors were exposed to.
- Avoid refined carbs (starches and sweets) which increase inflammatory mediators within minutes of consuming them, and are contributors to migraines
- Take probiotics.
- Increase omega 3’s and decrease omega sixes in the diet.
- RSD is due to an over activity of the sympathetic autonomic nervous system (SANS). Anything which can decrease SANS or it’s effects, or increase the parasympathetic autonomic nervous system (PANS) is likely to help this disorder. Any means of dilating blood vessels which are constricted due to sympathetic overdrive is likely to help.
- Mindfulness and meditation (as well as Yoga, and, I imagine, QiGong) are effective in decreasing SANS and increasing PANS.
- Counseling, Cognitive Behavioral Therapy (CBT).
- Low level laser treatments with settings and application to balance SANS and PANS.
- Any medication which causes slight or moderate somnolence (e.g., decreases sensory input)
- Amitriptyline (interestingly, one of my RSD patients has QT prolongation and another patient has heart rhythm problems, which makes me wonder if there are defects in the heart’s NMDA receptors—if there is such a thing.
- Benadryl
- Vistaril
- Benzodiazepines
- SSRI’s which are sedating
- Supplements which can be calming
- Amino acids
- GABA
- Glutamine
- Tryptophan
- 5 HTP
- Essential Oils
- Other botanicals
- Supplements to treat functional adrenal hyperfunction
- Ashwaganda
- Phosphatidyl serine (e.g., Seriphos)
- Adrenal calm or Catecholecalm
- Hormones which can be calming (this should be guided by hormone level testing)
- Progesterone
- DHEA-s
- Amino acids
- Treat other imbalances/disorders which are stressors which would increase sympathetic tone.
- Sleep apnea
- Depression (see our Functional Medicine approach to Depression and anxiety).
- Anxiety
- High Estrogen levels
- Low B12 or other low B vitamins (the B vitamins are depleted in stress, and then, once depleted, further aggravates the symptoms). B vitamins are important for nerve function (especially, vitamins B12, B6, and Folate). They are also important in phase one of detoxification in the liver (a metabolic process which makes toxic substances water soluble so that they can be excreted).
- Effects of heavy metals. I view heavy metals and petroleum products and plastics and pesticides as major players in any inflammatory process because they stay in the body for years, sometimes, and wreak havoc with many metabolic processes. Consider provoked urine test for heavy metals. Consider chelation, infrared sauna, and ionic foot baths and supplements to help unload these toxic substances.
- Avoid Substances/environmental stimuli which can increase sympathetic tone
- Monosodium Glutamate (MSG, Hydrolyzed vegetable protein), Aspartate / Aspartame / Nutrasweet
- Weight loss substances with stimulants (e.g., Ma Huang, Ephedra, caffeine)
- Video games, especially war games with violence, but all videogames can increase adrenaline / SANS.
- Electromagnetic Forces/Fields (EMF), from cell phones, cordless devices, living near power lines. See the book “Disconnect” to learn more about the effects of cell phones.
- Afrin nasal spray (oxymetazolone)
- Chocolate has theobromine and is a mild stimulant
- RSD is a migraine equivalent. Those of us who have been practicing for some time recognize that there is an increase of incidence of cephalgic migraines and migraine equivalents such as intestinal migraines. We have found that RSD always responds to one or another migraine treatment. Both (cephalic migraines and RSD) disorders appear to involve NMDA receptors. Both are neuroinflammatory autoimmune disorders. Both also are characterized by an over sensitivity of sensory nerves (cephalgic migraines are often brought on by –and exacerbated by–sensitivity to and stimulation of one of the sensory nerves [e.g., smell, vision, hearing, taste]). We have also found that interstitial cystitis (IC) is also a migraine equivalent: traditionally, we have used medications (e.g., amitriptyline) which are used in migraines for IC; it has responded to natural / alternative treatments used for migraines; it is characterized by hypersensitivity of nerves which suggest to the patient that he/she needs to evacuate the bladder even though the bladder is not really full (similar to the hypersensitivity of other migraines, but this time, involving the nerves of the bladder). Intestinal migraines are characterized by a hypersensitivity of sensory nerves in the GI tract, so that when a person eats even small amounts, there is abdominal pain. A list of treatments for migraines follows:
- Amitriptyline
- Propranolol
- Zomig (one of my RSD patients has a 40% decrease of his symptoms by taking Zomig, a migraine medicine every 2-3 weeks. He also does several other things to control the pain—see case histories below).
- Migraine cocktails: IV, IM, or oral. I often use this as a diagnostic maneuver. I give an IM migraine cocktail (60 mg of Toradol, 50 mg of Benadryl, and 4 mg of Zofran IM). We expect 8-12 hours of relief of pain w/ Toradol. If the pain relief lasts 18-24 hours or longer it increases our index of suspicion that the patient is dealing with RSD. I have one patient who takes oral Zofran, Benadryl, and Ibuprophen tid round the clock and has had significant decrease in his symptoms and the hair has been growing back on his legs (as is typical in this disorder, when the hair grows back it is much more course hair).
- Dehydration exacerbates all migraines and rehydration is part of treatment of all migraines.
- Regular dosing of anti-oxidants, in veggies, spices, chaga, etc.
- Anti-histamines, including Benadryl. Part of the way that the older anti-histamines work to decrease migraines, including RSD is that they make us drowsy (and thus decrease sensory input).
- Zofran used by itself is sometimes effective for migraines. It is a serotonin 5HTP-3c agonist and seems to be more effective than other anti-nausea meds for RSD. One of my patients is different and responds better to Phenergan than to Zofran, and I assume it is because Phenergan is more sedating for her.
- All standard advice for migraineurs applies to all people with migraine equivalents:
- Avoid cheddar cheeses, especially sharp cheddar cheeses.
- Avoid processed meats: bologna, salami, pastrami, pepperoni, sausage, hot dogs.
- Avoid foods high in nitrates, glutamates, and tyramine.
- Stay well-hydrated
- Allergy medications (often help, since part of the inflammatory response is a release of histamines and leukotrienes from eosinophils).
- Singulair / Montelukast (a leukotriene inhibitor).
- Antihistamines such as Benadryl, Zyrtec, Claritin, Vistaril.
- Other things which improve cellular function
- NAD.
- IV NAD was effective in decreasing symptoms in 3/3 of patients treated by Dr. Jeffrey Sturgess of Cour de Lane, Idaho. IV NAD, was also just as effective in treating Migraines, though the response was three weeks after the IV treatments.
- Nutrient-dense diet.
- E.g., a whole food plant-based diet, or Paleo diet. Especially important are the vegetables with their antioxidants and other phytonutrients.
- NAD.
- Anything to open/dilate arteries
- Nitric oxide (which is a vasodilator and acts as an anti-oxidant)
- Ozone. Rectal, IV, Ozone with UV blood therapy. At least 50% of RSD patients have decreased symptoms with rectal ozone. We have an Interstitial cystitis patient who responded to rectal ozone as well.
- IR sauna probably increases nitric oxide and also helps with detoxification.
- Exercise with oxygen, especially the program that alternates wind sprints on low oxygen with relaxed running on 100% oxygen. When we simulate altitude or do wind sprints, our nitric oxide level increases, which dilates blood vessels.
- Chelation, pulls out heavy metals but probably also increases nitric oxide.
- Cialis. Most of my male patients with RSD have significantly decrease pain and improved color of skin with daily Cialis. We prescribe 10 mg, take ½ qd. Recognize that there is risk of taking this in people with coronary artery disease.
- Bystolic and Coreg theoretically should help. Both of these medications are used to lower blood pressure and function partly by increasing nitric oxide which dilates blood vessels.
- Nitric oxide (which is a vasodilator and acts as an anti-oxidant)
- Conventional and alternative treatments for pain
- SNRI;s: Cymbalta. I avoid Effexor which is difficult to get off of/ discontinue.
- Amitriptyline
- Narcotics.
- Ultramm/Tramadol
- D phenylalanine (an amino acid which is a precursor for our endorphins).
- Acupuncture is relatively contraindicated, but use of the acupuncture meridians with a low level laser may be useful.
- Neurontin / Gabapentin, which makes patients drowsy, but also slows down conduction through the pain-conducting neurons.
- Sympathetic nerve blocks. This is often used as a diagnostic maneuver to diagnose RSD. If the patient responds with even a temporary decrease of pain, the patient probably has RSD.
- After the first few weeks or months it is usually not advisable to keep trying physical activity to normalize the function of the pain response. If the patient is getting worse instead of better with stimulation or exercise, or use of an extremity, then the activity should be stopped. My patient with the worst RSD, which is body-wide is in a wheelchair with an aluminum box to keep people from touching his feet which are the most sensitive part of his body affected by RSD.
- Control blood sugar: Insulin resistance is one of the most common causes of inflammation.
- IV ketamine, general anesthesia
- Ketamine Troches
Case Histories in RSD and Other Migraine Equivalents
NM: A man in his 60’s. Was injured at work.
Antecedents: Family history of Multiple Sclerosis, another neuro-inflammatory disorder. Personal history of…
Triggers: Trauma at work
Mediators: Trial of E stim—made sx’s worse. Sympathetic nerve block make symptoms worse.
Treatments:
- Sympathetic nerve block. Symptoms generalized to the rest of his body after this
- Antihistamines: Claritin, Vistaril
- Propranolol earlier—discontinued due to ___
- Singulair
- Exercise: PT, aquatic therapy
We have helped a lot of patients suffering with CRPS and as you see above, there is much that can be done. If you would like to work with us to help alleviate your symptoms you suffer from with RSD or CRPS, please give us a call at (801) 228-1906. We are happy to do a free phone consultation to discuss whether or not you are a candidate for our treatment, and we are excited to help any and all those suffering with CRPS to find relief and take back their life.